Table of Contents
What is Thalassemia?
Thalassemia is a group of inherited hemolytic anemia disorders, is characterized by reducing or absent amounts of hemoglobin. The oxygen-carrying protein inside the red blood cell this condition causes a varying degree of anemia.
It’s Defective the synthesis in the polypeptide chains of the protein component of hemoglobin or decreased the production of hemoglobin, a molecule found inside all red blood cells that transport the oxygen through the body
It is a pathophysiological hereditary disease common in any part of the resulting from the defect in the synthesis of the red blood pigment hemoglobin also called Cooley anemia.
The production of one or more globin chain within the Hb molecules is reduced leads to
- Hypocromia – Hypo-less, Cromia-Color means an abnormal decrease in the Hb content of RBC.
- Extreme Microcytosis – Small than Normal RBC.
- Hemolysis – Destruction of Red Blood Cell.
It is caused by variant or missing genes that affected how people’s bodies make Hemoglobin. People with thalassemia make less hemoglobin and less circulation of red blood cells than normal, resulting in mild and severe anemia.
It can cause complications to include iron overload bone deformities and cardiovascular illness. However, this same inherited disease of red blood cells may confer a degree of protection against malaria.
Types Of Thalassemia
The two main type
- ALPHA
- BETA
They are the two protein chains that help to make up normal hemoglobin. Hemoglobin includes two kinds of protein chains first is the alpha-globin chain and the second one is the beta-globin chain. In case the problem is creating by the alpha-globin so it called alpha-globin thalassemia and in case the problem is facing by the beta-globin so it called beta-thalassemia.
Alpha
Alpha patient hemoglobin does not produce enough protein this type is commonly found in southwest Asian India. To make alpha globins’ protein chain we need for a gene to each chromosome 16 we get two from each process it at least the gene is missing produces alpha thalassemia.
Beta
Beta needs two globin genes to make globins’ chain we get one from each parent it two of these genes are facility produces beta. There are divided into Three-Part.
- Beta Minor
- Beta Major
- Beta Intermediate
1.Beta Thalassemia Minor
If one gene is affected a person is a carrier and has mild anemia. The condition is called beta trait or beta thalassaemia minor, Beta minor often goes undiagnosed because kinds with the condition have no real symptoms other than mild anemia and small red blood cell. It is often suspected based on routine blood tests such as a completed blood count (CBC) and can be confirmed with a hemoglobin’s electrophoresis.
2.Beta Thalassemia Major
Beta is also called coolly anemias is a severe condition in which regular blood transfusion is necessary for the child to survive. People with this disease accumulate deposits of iron especially in the liver heart and endocrine glands. The deposit eventually can affect the normal functioning of the heart and liver in addition to delaying growth and sexual maturation.
3. Beta Thalassemia Intermideat
Beta intermedia disease having a varying type of effect on children. Mild anemia can be their symptoms or they can slightly require a regular blood transfusion.
Causes of Thalassemia
Genetic – Most alpha syndrome results from genetics clinical heterogeneity. the thalassemias syndrome caused by a replacement of the heterogeneity of mutation.
Hemoglobin – Adult has mainly hemoglobin made up of two alpha two beta chains together with Hb alpha 2<2% (2alpha and 2 betas).

- There are two alpha genes located on the chromosome and two beta genes on the chromosome.
- At birth, Hbf accounts for 70-90% in a normal individual, and gamma chain synthesis’ is only reflected beta chain gradually.
- Impairment of beta synthesis leads to the patient being asymptomatic at birth.
You also Read This the Details Dyspenea (Shortness of breath).
Symptoms
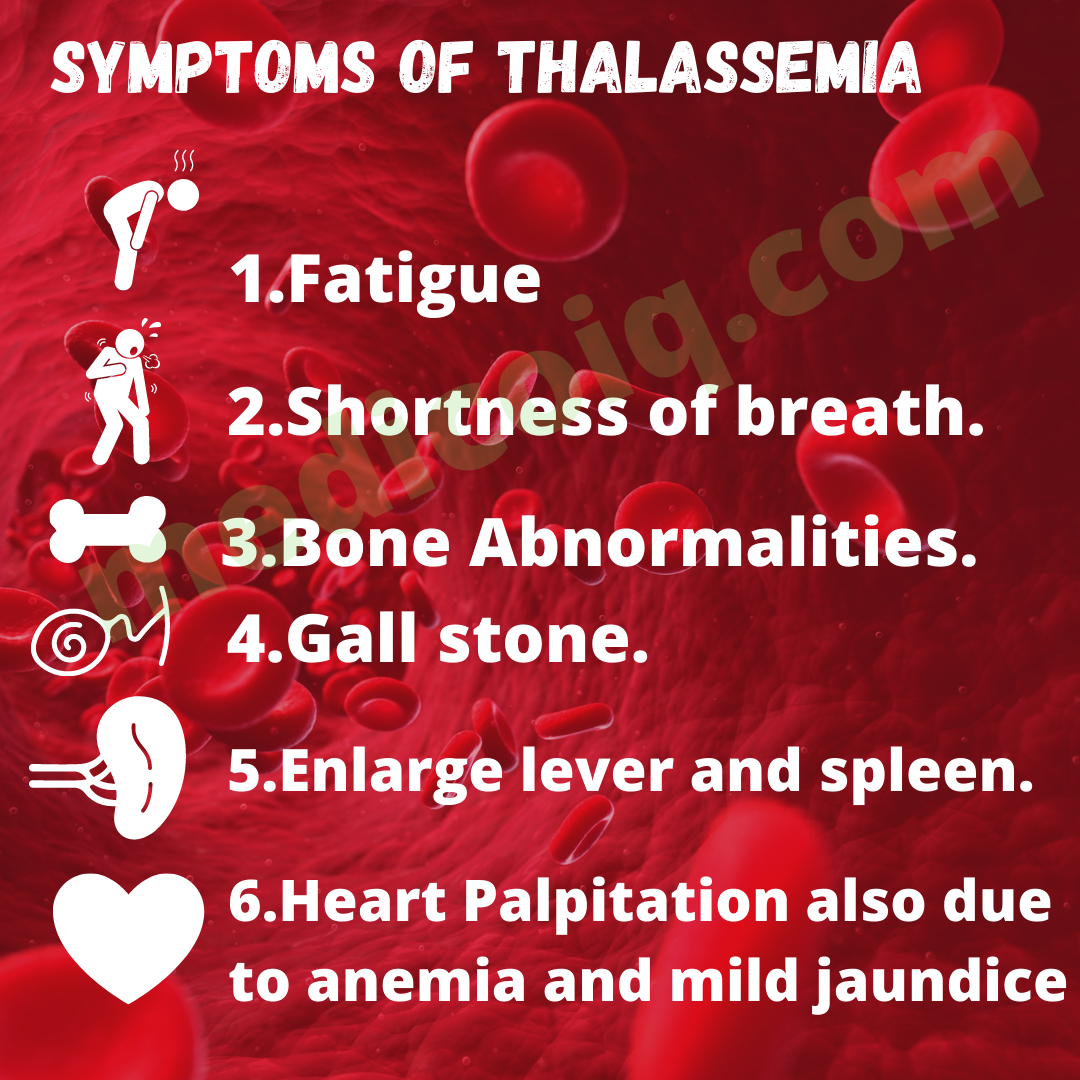
The symptoms of these diseases are depended upon the type of the disease.
1.Mild Anemia– People who have alpha or beta characteristics can have mind anemia. this type of thalassemia have nosing and symptoms in many people
2.Mild to moderate anemia and other sing and symptoms – People who have beta-thalassemia intermedia have mild to moderate anemia. they also have other health problems such as.
- Fatigue.
- Shortness of breath.
- Bone Abnormalities.
- Heart Palpitation also due to anemia and mild jaundice.
- Gall stone.
- Enlarge lever and spleen.
3.Sever Anemia and other Singh and symptoms – People with beta major have severe thalassemia. Sing and symptoms occur within the 2 years of life they many include severe anemia and other serious health problem such as
- Pale and listless appearance
- Poor Appetite
- Enlarge liver, heart, and spleen
- Dark urine
- Jaundice
- Bone problem
- Bleeding tendencies
- frequent infection
Diagnostic Test
Manly the diagnosis of this disease using blood tests, including complete blood counts and special hemoglobin tests.
- History taking
- Physical examination
- Complete blood count- CBC Provide the amount of hemoglobin and the different kinds of blood cells, such as red blood cells, in a sample of blood. in this method measure hemoglobin levels in quantities of red blood cells their size or other elements.
- Reticulocyte count –this blood cell test measure how fast red blood cell is being made the bone marrow and released into the blood.
- Iron –studies of iron will help the doctors determine the anemia.
- The genetic test-DNA analysis will help the diagnosis of this disease.
Treatment
Treatment for this disease depends on the type or type of disease. Generally, doctors use three standard treatment for a moderate and severe form of thalassemia such as
-
- Blood transfusion
- Iron-chelating therapy
- Folic acid supplement
- Blood transfusion – A blood transfusion given through a needle in a vein and gives a healthy blood cell with normal hemoglobin if the patient has beta major or coolly anemia needs a regular blood transfusion (after every 2-4weak).
- Iron chelating agent– The hemoglobin in red blood cell is an iron-rich protein regular blood transfusion can lead to a build-up of iron in the blood .this condition is called iron overloaded it damage the liver heart and another part of the body.
- Folic acid supplements – Folic acid is a B-vitamin that helps build healthy red blood cell patient may need to take folic acid supplements in addition to blood transfusion and iron-chelating therapy.
- Blood and marrow stem cell transplant- In this method replace abnormal or faulty stem cells with healthy ones from another person .stem cells are the cell inside bone marrow that make red blood cells and other yep of blood cells .the stem cell transplant is the only treatment that can cure thalassemia.
- Surgery – Surgery may be needed when body organs, such as the spleen or gall bladder are affected.
- Other Treatment – People with severe thalassemia are more likely to get an infection that can worsen their anemia. they should get an annual flu shot and the pneumonia vaccine to help prevent infection.
FAQ
-
Can thalassemia be cured?
The stem cell transplant is the only treatment that can cure thalassemia. Blood and marrow stem cell transplant- In this method replace abnormal or faulty stem cells with healthy ones from another person .stem cells are the cell inside bone marrow that make red blood cells and other yep of blood cells
-
How is thalassemia detected?
History taking
Physical examination
Complete blood count
Reticulocyte count
Iron
The genetic test -
What blood type is thalassemia?
Thalassemia is a group of inherited hemolytic anemia disorders, is characterized by reducing or absent amounts of hemoglobin. The oxygen-carrying protein inside the red blood cell this condition causes a varying degree of anemia.
They are two main types 1.Beta thalassemia, 2.Alpha Thalassemia -
How long do thalassemia patients live?
Mainly Thalassemia patient live up to 25-30.if they under improve facility so they live up to 60 year







